Background: Allogeneic HSCT for adult patients with sickle cell disease (SCD) is potentially curative but not commonly utilized therapy due to complications such as graft failure (GF) and organ toxicity. At our center, we adopted a non-myeloablative (NMA) conditioning regimen in adult patients with severe SCD. Herein, we are reporting our outcome data of up to 5-years of follow up post HSCT.
Methods: Following IRB approval, adult patients that underwent HSCT from 2015 to 2020 for severe SCD with at least 6 months of follow up were included. Indications for HSCT were; presence of recurrent vaso-occlusive crisis (VOC), end organ damage, multiple joint AVN, recurrent priapism, transfusion dependency, or RBC alloimmunization. Conditioning regimen consisted of alemtuzumab (1 mg/kg divided over 5 days on days -7 to -3) and 300 cGy TBI on day -2 or -1. Pre-transplant preparation consisted of Hydroxyurea at maximum tolerated dose for 2-3 months. Peripherally mobilized stem cells targeting 10x106/kg of CD34 cells were used. For GVHD prophylaxis sirolimus was started on day -1 and continued for one year with tapering off if lymphoid chimerism is > 50%. EFS was defined as time from HSCT to graft failure or death from any cause whereas OS was defined as time from HSCT to death or last documented follow up.
Results:
A. Baseline Characteristics:
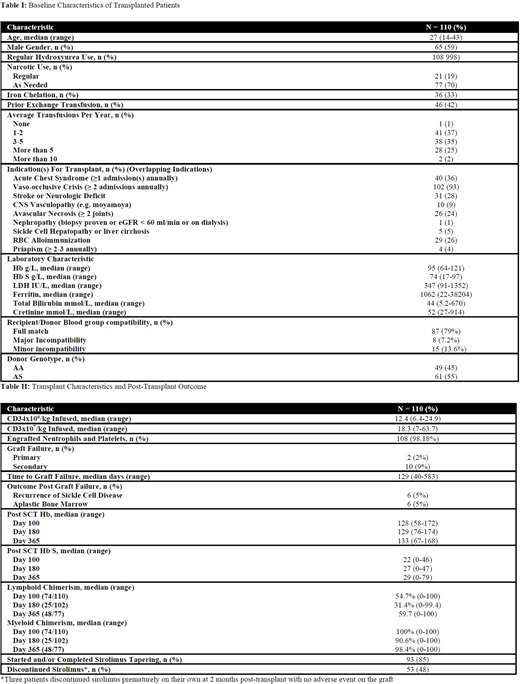
A total of 110 patients were included with a median (range) age of 27 years (14-43), 59% of patients were male. Baseline median hemoglobin and hemoglobin S (HbS) was 95 g/L (64-121) and 74 % (17 -97), respectively. Regular hydroxyurea use was among 108 (98%) and 109 (99%) of patients required at least ≥ 1 transfusion annually. Narcotic pain killers were used regularly in 21 (19%) of patients. Median pre-HSCT ferritin was 1062 and iron chelation was used in 36 (33%). The most common indications for HSCT were (overlapping) recurrent VOC in 93%, ACS in 36%, stroke in 28% and RBC allo-immunization in 26%. Furthermore, 18 patients had 3 indications, 45 had 2 indications while the remaining 47 patients had one indication. Furthermore, 10 (9%) patients had Moya-Moya disease, 5 (5%) had sickling hepatopathy and or liver cirrhosis with total bilirubin up to 670 mmol/L and 1 (1%) patient had end stage renal disease on peritoneal-dialysis. A total of 61 (55%) donors were SC trait and underwent GCSF mobilization without major adverse events as previously reported (Damlaj et al., BMT 2018). 8 (7%) and 15 (14%) had major and minor ABO incompatibility, respectively. The remaining characteristics are found in table 1
B. Transplant Characteristics and Post HSCT Outcome:
Median infused CD34x106/kg was 12.4 (6.4-24.9) and 108 (98%) patients had successful engraftment. A total of 12 patients experienced GF; 2 as primary and 10 as secondary within a median time of 129 days (40-583). Outcome post GF was as follows; recurrence of SCD in 6 (50%), aplastic bone marrow in 6 (50%) of whom 4 underwent a second allogeneic HSCT with Flu-Cy-ATG platform and all from MRD. Among second HSCT recipients, 3 are still alive and in SCD free disease status. Among patients with GF, 5 (42%) had minor ABO incompatibility while the remaining 7 (58%) were ABO matched HSCT.
Mild acute skin GVHD (grade I to II) occurred in 3 cases and 4 cases developed autoimmune haemolytic anemia that resolved with steroids. Only one patient had CNS bleeding 2 years post-transplant in a background of history of stroke and Moya-Moya disease. A total of 53 (48%) patients successfully discontinued sirolimus while an additional 40 (35%) are on active taper. There were a total of 4 successful pregnancies in 3 patients; 3 pregnancies completed to term while 1 miscarried. Median follow up for the cohort is 16.8 (2-66) months. Estimated 2-year EFS and OS was 87.3% (+/- 0.036) and 97% (+/-0.017). All deaths were due to GF. There was no difference in outcome (EFS or OS) between patients receiving graft from normal vs. SC trait. Post HSCT Hb and chimerism results are shown in table 2.
Conclusions:
Herein, we present a large real-life experience demonstrating feasibility and favourable outcome of NMA HSCT in adult patients with severe SCD including patients with significant organ dysfunction or neurologic vasculopathy. Successful pregnancies and long-term discontinuation of immune suppression was possible. Longer follow up is warranted to ascertain stability of graft function over time.
Disclosure: The authors declare they have no relevant conflicts of interest
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal